How Physiotherapy Helps In Slipped Disc And Sciatica Pain?
In my clinic, patients often arrive saying one of three things:
- “Doctor, my MRI shows a slipped disc — will I need surgery?”
- “I have sciatica pain shooting down my leg. Is physiotherapy safe?”
- “Someone told me rest is better. Someone else told me exercise is better. I’m confused.”
This confusion is understandable. Slipped disc and sciatica are widely discussed online, but rarely explained clearly or honestly.
Let’s slow this down and explain it the way I would in a real consultation.
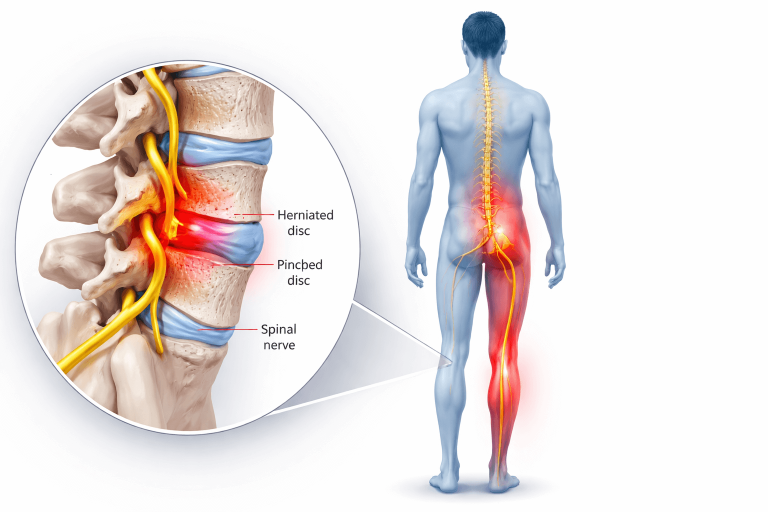
What exactly is a slipped disc and how is it linked to sciatica?
A slipped disc (more accurately called a disc bulge or disc herniation) happens when the soft cushion between the spinal bones loses its normal position or shape. This becomes a problem only when it irritates or compresses a nearby nerve.
That nerve irritation is what causes sciatica pain — typically:
- Sharp or burning pain from lower back to buttock and leg
- Tingling, numbness, or heaviness in the leg
- Pain that worsens with sitting, bending, coughing, or sudden movements
Important clinical point:
Not all disc bulges cause pain. Many MRI findings are incidental. Treatment decisions should be based on symptoms and function, not scans alone.

Why physiotherapy is often the first and best line of treatment
From a clinical perspective, most slipped disc and sciatica cases are mechanical and functional problems, not surgical ones. Physiotherapy helps by addressing why the nerve is irritated, not just masking pain.
Physiotherapy works on 4 key levels
1. Pain calming and nerve protection (early phase)
In the acute phase, the goal is not aggressive exercise.
What we focus on:
Reducing nerve irritation
The first goal is to calm the irritated nerve by reducing pressure and inflammation around it. This helps ease leg pain, tingling, or burning sensations and creates a safer environment for healing before active exercises begin.
Finding pain-relieving positions
Certain positions naturally reduce stress on the spine and nerves. We help patients identify postures for sitting, lying, and resting that ease pain and prevent unnecessary strain during daily activities.
Teaching safe movement strategies
Instead of avoiding movement, patients learn how to move safely without worsening symptoms. This includes guidance on bending, getting up, walking, and changing positions in ways that protect the spine and reduce fear of movement.
This may include:
Gentle positioning techniques
Simple, supported positions are used to reduce stress on the spine and calm irritated nerves. These positions help ease pain during rest and allow the body to settle before progressing to movement or exercise.
Activity modification (what to avoid, what is safe)
Patients are guided on which movements or activities may worsen symptoms and which are safe to continue. This prevents unnecessary flare-ups while keeping the body active enough to support recovery.
Manual therapy only if clinically appropriate
Hands-on treatment is used selectively, based on symptoms and examination findings. It is never forced and is avoided if it risks increasing nerve irritation or discomfort.
Education to reduce fear and guarding
Understanding the condition helps patients move with confidence rather than fear. Clear explanations reduce protective stiffness and tension, which often worsen pain and slow recovery.
What doesn’t help here:
Blind stretching, forceful massage, or random YouTube exercises often worsen symptoms.
2. Restoring movement without aggravating the disc
Once pain starts settling, we gradually restore controlled spinal movement.
Why this matters:
Prolonged rest stiffens the spine
Staying in bed or avoiding movement for too long causes the spine and surrounding muscles to become stiff and weak. This stiffness can actually increase pain and make returning to normal activity more difficult.
Fear-based avoidance delays recovery
When pain leads to fear of movement, people often stop using their body normally. This protective behavior can prolong symptoms by increasing muscle tension, weakness, and sensitivity around the spine.
Discs heal better with guided movement, not immobility
Spinal discs receive nourishment through movement, not rest alone. Carefully guided exercises and daily activities help support healing while protecting the nerve, whereas complete immobility can slow recovery.
Physiotherapy helps you:
- Move without triggering leg pain
- Learn safe bending, sitting, and getting up
- Improve spinal mobility within pain-free limits
This stage is where many patients start regaining confidence.
3. Addressing the real cause: load, posture, and muscle control
In my clinical experience, sciatica rarely happens “out of nowhere.”
Common contributing factors:
Poor core and pelvic control
When the deep muscles that support the spine and pelvis are not working well, the lower back takes extra strain. Over time, this lack of control can increase stress on spinal discs and surrounding nerves.
Prolonged sitting or improper work posture
Sitting for long hours, especially with poor posture, increases pressure on the lower back and discs. Without regular movement or support, this can gradually trigger or worsen back and leg pain.
Weak hip and trunk muscles
The hips and trunk help absorb load during daily movements like walking, bending, and lifting. If these muscles are weak, excess force is transferred to the lower back, increasing the risk of pain and injury.
Sudden overload without preparation
A sudden increase in activity, lifting, or exercise without gradual conditioning can overload the spine. This often leads to flare-ups because the body has not had time to adapt safely.
Physiotherapy focuses on:
- Core stabilization (not just abs, but deep control)
- Hip and pelvic mechanics
- Gradual load tolerance
- Postural correction for daily life
👉 This is what prevents recurrence, not just short-term relief.
4. Gradual return to normal life (work, walking, exercise)
A successful physiotherapy program does not end when pain reduces.
We guide patients through:
- Return to work planning
- Sitting and desk ergonomics
- Walking progression
- Gym or activity reintroduction (if appropriate)
This phase is crucial. Many relapses happen because patients stop therapy too early or return to activity without guidance.
A realistic clinical example
A 42-year-old office professional came with severe leg pain and MRI-confirmed L4-L5 disc herniation. He was afraid to bend or walk, convinced surgery was inevitable.
Treatment approach:
- First 2 weeks: pain control, nerve unloading positions, movement education
- Weeks 3–5: controlled mobility + core and hip stability
- Weeks 6–8: posture correction, work modification, endurance training
Outcome:
- Leg pain reduced significantly
- Returned to work without surgery
- Learned how to manage future flare-ups safely
This is a common, realistic recovery timeline, not an exception.

When physiotherapy may Not be enough
Honest medicine means knowing limits.
Physiotherapy alone may not be sufficient if there is:
- Progressive leg weakness
- Loss of bladder or bowel control
- Severe numbness worsening over time
- No improvement despite consistent, correct therapy
These situations require urgent medical or surgical evaluation.
Red flags patients should never ignore
Seek immediate medical attention if you notice:
- Sudden loss of bladder or bowel control
- Numbness in the groin or saddle area
- Rapidly increasing weakness in the leg
- Unrelenting night pain or unexplained weight loss
These are not physiotherapy problems — they are medical emergencies.
Common home mistakes that delay recovery
From daily practice, these are frequent issues:
- Complete bed rest for weeks
- Self-manipulation or forceful stretches
- Ignoring leg pain and “pushing through”
- Following generic exercise videos without assessment
- Stopping therapy as soon as pain reduces
Recovery requires guidance, not guesswork.

When should you start physiotherapy?
In most cases:
- Early, guided physiotherapy is safer than waiting
- Starting within the first few weeks often leads to faster recovery
- Delaying treatment increases fear, stiffness, and dependency on medication

How long does recovery realistically take?
This varies, but clinically:
- Mild cases: 3–4 weeks
- Moderate cases: 6–8 weeks
- Chronic or recurrent cases: longer, with phased goals
Physiotherapy is not a one-day fix — it’s a process of restoring function safely.
Final thoughts from a clinician
Slipped disc and sciatica pain can be frightening — but they are not automatic surgery diagnoses.
When done correctly, physiotherapy:
- Respects tissue healing
- Reduces nerve irritation
- Restores confidence and movement
- Lowers recurrence risk
The key is individual assessment, clinical reasoning, and patient education — not aggressive treatment or unrealistic promises. If you’re unsure whether physiotherapy is right for your condition, a proper evaluation can help you make a safe, informed decision.